The following is provided as published in the Australian Veterinary Journal, Volume 95, Number 8, August 2017. The information in the disease bulletin was correct at the time of publication.
Author: Ben O’Toole, On Plant Veterinarian (Department of Agriculture, Water, and the Environment).
Sheep and goat pox
Sheep pox and goat pox are highly contagious diseases that affect small ruminants. Clinical signs include fever, papules and pustules (rarely vesicles) on sparsely woolled or haired skin, hypersalivation and ocular and nasal discharge.1 Sheep pox and goat pox are listed as notifiable diseases by the World Organisation for Animal Health (OIE) and are enzootic in parts of Africa north of the equator, the Middle East, Turkey, Afghanistan, Pakistan, India, Nepal, parts of China, Bangladesh and Vietnam and have recently made frequent incursions into southern Europe.2 Australia is free of sheep pox and goat pox and has never had a reported case.1 Susceptibility to the disease is dependent on factors such as breed, level of immunity, age of the animal and the strain of the virus3 and it is possible that the naïve sheep and goat populations in Australia may experience high morbidity and mortality if sheep pox and goat pox were introduced. The Australian Veterinary Emergency Plan (AUSVETPLAN) disease strategy for sheep pox and goat pox suggests that an uncontrolled outbreak in Australia would result in serious stock losses for the sheep and goat industries and continuing economic loss may occur if an epidemic were to develop.1
Aetiology
Sheep pox virus and goat pox virus are members of the Poxviridaefamily of viruses, which are within the genus Capripoxvirus and are also closely related to lumpy skin disease virus of cattle. Sheep pox and goat pox viruses were once thought to be strains of the same virus; however, advances in genetic sequencing have demonstrated that they are separate viruses.2 Sheep pox and goat pox viruses are usually host specific, but some strains have been shown to infect both sheep and goats. Recombination can also occur between sheep and goat strains, resulting in a wide range of intermediate host preferences and virulence.2
Transmission
Once an animal is infected, the virus can be present in ulcerated papules on mucous membranes prior to causing necrosis, as well as being present in saliva, nasal and ocular secretions, faeces, urine, milk, and skin lesions under scabs.2 The most common mode of transmission is the respiratory route, following close contact between infected and susceptible animals. Contact with skin abrasions or mucous membranes are other methods of transmission, as well as indirect transmission via fomites and mechanical transmission via insects.2 Movement of infected animals is the main method by which sheep pox and goat pox viruses are spread into new areas.1

(Source: CSIRO and the Canadian Food Inspection Agency (CFIA), National Centre for Foreign Animal Disease, Winnipeg, Canada)
Clinical disease
The incubation period for sheep pox and goat pox ranges from 4 to 14 days, but is usually around 12 days.1 Affected animals have an initial fever, which is usually followed 1–5 days later by the development of characteristic skin lesions (Figure 1).4 Skin lesions consist of erythematous macules, which develop into hard papules of 0.5–1.5 cm diameter.4 In the more common form of the disease (papulovesicular), the papules develop depressed, whitish grey and necrotic centres with a surrounding area of hyperaemia.4 Rarely, papules may be covered with fluid-filled vesicles.2 In the uncommon nodular form, also known as ‘stonepox’, the papules develop into nodules.4 Sheep pox and goat pox lesions tend to develop on areas of thinly woolled or haired skin such as the face, ears, axillae, groin, perineum and under the tail. They can take several weeks to heal and may result in the development of permanent scars. Animals are also susceptible to fly strike and secondary bacterial infections during the healing process.4

(Source: CSIRO and the Canadian Food Inspection Agency (CFIA), National Centre for Foreign Animal Disease, Winnipeg, Canada)
Enlargement of all superficial lymph nodes can also occur, usually within a day of the appearance of generalised papules.4 Lesions may also be present on mucous membranes (Figure 2) and internal organs. Lesions in the nares, mouth, eyes or eyelids can lead to hypersalivation, inappetence and conjunctivitis.4 Papules or ulcerated papules are also commonly seen in the abomasal mucosa and may also be seen in the rumen, large intestine, pharynx, trachea and oesophagus.4 Animals with lung lesions may develop respiratory signs such as coughing, nasal discharge and dyspnoea.4 Lesions in the lungs generally consist of congested, oedematous or consolidated areas with firm grey or white nodules that can be up to 5 cm in diameter.4
Peracute cases of sheep pox and goat pox may show few clinical signs before sudden death. Postmortem findings would include signs consistent with septicaemia, as well as hyperaemic lungs with typical pox lesions5 (Figure 3).
Because the sheep and goat population in Australia is naïve to sheep pox and goat pox, it is likely that the initial signs of an outbreak would be animals suffering from the ‘septicaemic’ form of the disease with a high morbidity and mortality rates, with deaths possibly occurring before the development of skin lesions.5
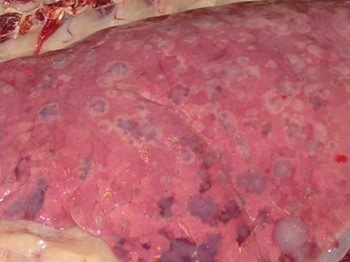
(Source: CSIRO and the Canadian Food Inspection Agency (CFIA), National Centre for Foreign Animal Disease, Winnipeg, Canada)
Morbidity and mortality
Morbidity and mortality rates in sheep and goats vary according to breed, level of immunity, age of the animal and the strain of the virus.3 In enzootic areas, morbidity can vary from 1% to 75% for indigenous breeds4 and mortality can range from 5% to 10%.2 It has been reported that European or Australian breeds of sheep and goats are more susceptible to the disease when they are introduced into enzootic areas, and morbidity and mortality can approach 100%.2
Diagnosis
Sheep pox and goat pox should be considered in cases where there is high morbidity and mortality in sheep and goats, and where typical pox lesions are seen on the skin and respiratory and digestive mucosa. Differential diagnoses include contagious pustular dermatitis (scabby mouth), bluetongue, mycotic dermatitis, ectoparasites and photosensitisation.1
A tentative diagnosis can be made rapidly using electron microscopy because of the characteristic morphology of capripoxviruses. Histopathology can also be useful, with extensive inflammatory, necrotic and proliferative changes as well as the presence of Borrel cells (infiltrating epithelioid cells) and intracytoplasmic inclusion bodies being seen in pox lesions.1
Confirmatory diagnosis is made by specifically identifying the virus in tissues by virus isolation, in addition to detecting viral DNA in tissue samples using PCR techniques.1
Specimens required for testing are summarised in Table 1 and include biopsies of skin, respiratory and gastrointestinal lesions (fresh and fixed), nasal swabs and whole blood collected in EDTA tubes.1 Samples should be sent to the state or territory diagnostic laboratory as soon as possible, where they will be forwarded to the Australian Animal Health Laboratory in Geelong, Victoria.1
Blood samples and unpreserved tissue specimens should be chilled and transported on water ice or frozen gel packs. Freezing of samples below –20°C should be avoided because it reduces the sensitivity of some diagnostic tests. If the journey is expected to take several days, the specimens should be sent on dry ice.
| Specimens | Diagnostic test |
|---|---|
| EDTA blood: (7–10 mL/animal) from live, clinically affected animals | Agent detection |
| Nasal swabs: from live, clinically affected animals | Agent detection |
| Fresh tissue: characteristic pox lesions from skin as well as respiratory and gastrointestinal tracts (2g of each tissue) | Agent detection |
| Fixed tissue: characteristic pox lesions from skin as well as respiratory and gastrointestinal tracts (in neutral-buffered formalin). | Histopathology |
Prevention and control
There is no treatment available for sheep pox and goat pox, apart from supportive therapy. In countries where sheep pox and goat pox are enzootic, vaccination can be used as a method of control in combination with other sanitary measures such as culling, isolation of infected herds, proper disposal of cadavers, stringent cleaning and disinfection, quarantine and movement controls.2
Several attenuated vaccines are available and can confer an immunity that lasts up to 2 years.2 Inactivated vaccines are also available but may only provide short-term immunity.
Significance to Australia
The possibility of sheep pox or goat pox entering Australia via movement of infected animals is remote because Australia does not permit the importation of live sheep or goats or their semen or embryos from countries in which sheep pox and goat pox are enzootic. However, sheep pox and goat pox viruses are relatively environmentally stable and are readily transported on fomites. Indirect contact is an important means of spread and the most likely scenario of sheep pox and goat pox being introduced into Australia is via contaminated fomites and animal products. Examples include returning sheep transport vessels, clothing, equipment and unprocessed wool products introduced by people travelling from enzootic areas.1
If an outbreak of sheep pox or goat pox occurred in Australia, the economic impact would be potentially significant for Australia’s sheep and goat industries, with losses resulting from death of livestock, the cost of control or eradication, and loss of international market access.
Australia’s response policy is to eradicate sheep pox and goat pox in the shortest possible timeframe using elimination, reinforced by a combination of strategies such as sanitary disposal, quarantine and movement controls, decontamination of fomites, tracing and surveillance, zoning and an awareness campaign.1 It would then take 6 months after the destruction of the last affected animal for Australia to be declared free of the disease. Australia would also be required to undertake a disease surveillance program during this period.
If sheep pox or goat pox were to become enzootic, economic losses from the loss of animals and cost of preventative vaccination would occur, as well as a permanent loss of some export markets. The loss of Australia’s major wool, goat fibre and skin markets could also be a potential consequence.1 Therefore, it is essential that control and eradication measures are taken immediately to prevent this from occurring.
Veterinarians play an important role in the early detection of the disease, which is critical for effective disease control. Sheep pox and goat pox are nationally notifiable diseases and any suspected outbreak must be reported to state or territory veterinary authorities.
The Emergency Animal Disease Watch Hotline can also be contacted on 1800 675 888.
References
1. Animal Health Australia. Australian Veterinary Emergency Plan (AUSVETPLAN). Disease strategy: sheep pox and goat pox (Version 3.1). AHA, Canberra, ACT, 2011.
2. Fernandez PJ, White WR. Atlas of transboundary animal diseases. Revised edn. OIE, Paris, 2016;232–238.
3. United States Department of Agriculture. Sheep and goat pox standard operating procedures. 1: overview of etiology and ecology. USDA, Riverdale, Maryland.
4. The Centre for Food Security and Public Health. Sheep & goat pox: Capripoxvirus infection. Iowa State University, Ames, Iowa. Accessed April 2017.
5. Watt B, Scrivner C. Sheep and goat pox. Flock and Herd case notes (originally published in Skirting the Issues, official newsletter of the Australian Sheep Veterinarians, Autumn 2014;6–9). Accessed April 2017.
The images are from in vivo challenge experiments that were conducted by CSIRO and the Canadian Food Inspection Agency (CFIA) at the National Centre for Foreign Animal Disease (Winnipeg, Canada) during a collaborative project to enhance the diagnostic capability for the diseases caused by capripoxviruses. This work was supported by the Australian Woolgrowers and the Australian Government through Australian Wool Innovation Limited Project No. EC145, as well as by CFIA Quickstart grants QSW0505 and QSW0503, and CFIA RPS W0309.
